Research Projects
There is increasing evidence from epidemiological and preclinical studies about the effects of environmental factors, such as early-life and chronic stress, as well as traumatic experiences, on microglia biology. These factors may play a role in determining an individual's susceptibility to psychiatric and neurodegenerative diseases. However, the precise molecular mechanisms that govern the interaction between neuronal stress circuits and the immune system are still not fully understood. Previous studies have indicated that exposure to stress can increase the risk of disease by promoting inflammation both in the body and in the brain. This inflammation, and consequently the risk for disease, may be influenced by genes and pathways that respond to stress and regulate immune function. A critical element in this process is secretory autophagy. Unlike traditional autophagy, this non-lytic form of cellular waste management is essential for the release of vesicular contents, including pro-inflammatory cytokines such as Interleukin-1ß. The role of known secretory autophagy regulators, FKBP5 and SKA2 – both stress-responsive genes associated with psychiatric disorders – underscores its significant role in mediating the interactions between neuronal stress circuits and the immune system. In our lab, we use cellular assays and mouse models to explore the detailed workings of secretory autophagy at the molecular level. Specifically, we study how chronic stress affects neuroinflammation and behavior, focusing on what happens when secretory autophagy is either disrupted or excessively activated. The insights gained from this research are crucial for a deeper understanding of the molecular mechanisms underlying stress-related psychiatric and neurodegenerative diseases.
Secretory Autophagy: A Molecular Bridge between Stress and Neuroinflammation
Exploring the Gut-Brain axis: Advancing Microbiome-Based Interventions for Stress-Related Disorders
The gut microbiome is increasingly recognized not only as a crucial player in the body's physiological homeostasis but also in pathophysiological disruptions. Studies suggest that the gut microbiome plays a key role in stress responsiveness and affective disorders, including anxiety and major depressive disorder (MDD). However, its specific role in posttraumatic stress disorder (PTSD) remains to be fully understood. Furthermore, research indicates that diets targeting microbiota and specific bacterial strains may positively influence mood, anxiety, cognition, stress, and hypothalamic-pituitary-adrenal (HPA) axis function. Consequently, therapeutics based on the microbiome hold significant promise for the treatment of mental disorders. A major challenge in this field is the incomplete understanding of the relationship between the gut microbiome and psychopathology, which hampers the rational development of microbiome-based therapeutics for preventing or alleviating stress-related psychiatric disorders, including PTSD. Our research aims to address this knowledge gap by investigating the impact of stress exposure on the gut microbiome and the brain, using mouse models of stress. Additionally, we are examining whether specially designed microbiome-based interventions can enhance stress resilience in mice. Our research is poised to provide critical insights for future studies on microbiome-targeted interventions, aimed at preventing or mitigating PTSD and its detrimental effects on physical health.
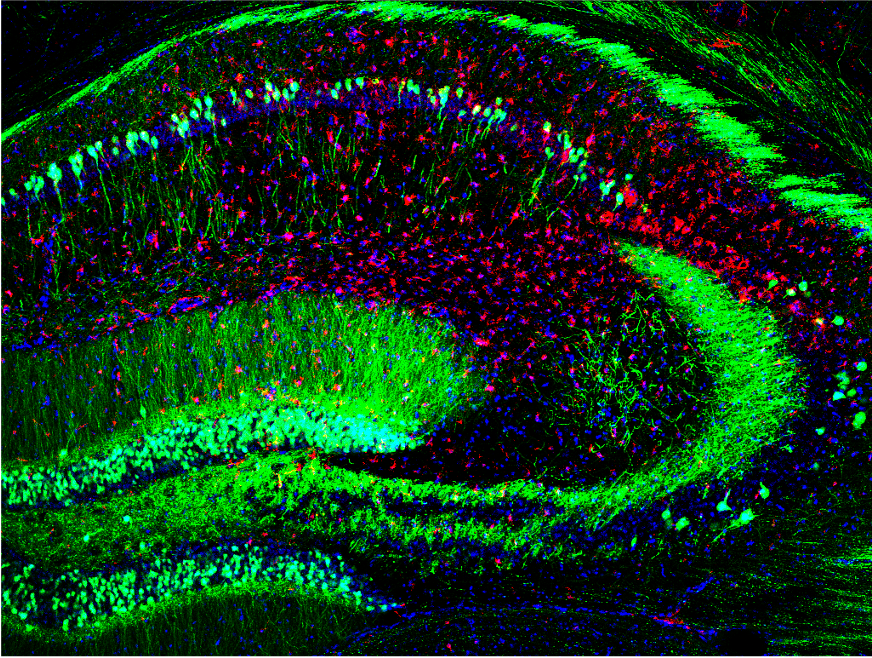
Decoding Sex Differences in Stress Resilience: A Focus on the Bed Nucleus of the Stria Terminalis
While mood and anxiety disorders are known to be twice as prevalent in women compared to men, the underlying sex-specific mechanisms in affective disorders remain largely unexplored. One critical brain region, the bed nucleus of the stria terminalis (BNST), plays a pivotal role in stress response and in regulating emotional and social behaviors. Yet, its potential sex-specific dysregulation in mental disorders has not been thoroughly investigated. Our research aims to help fill this gap by examining sex-specific gene networks within the BNST that influence susceptibility and resilience to stress. We employ single-cell transcriptomics in animal models, combined with chemogenetic approaches, to uncover these mechanisms. Our goal is to identify novel targets for the development of pharmaceutical interventions tailored to treat mental disorders in humans, with a particular focus on addressing gender disparities in these conditions.
Deciphering SKA2's Impact on Bipolar Disorder and the Stress Response in the Brain
Stress-related psychiatric disorders, such as bipolar disorder (BD), present a significant global burden, with their underlying molecular mechanisms still not well understood. A key regulator of the stress response in mammals is the hypothalamic-pituitary-adrenal (HPA) axis, which controls the stress-induced release of glucocorticoids. Aberrant glucocorticoid release due to chronic stress or traumatic experiences can harm the brain, increasing vulnerability to mental disorders. Therefore, disturbed activation or regulation of the body’s stress response through the HPA axis is a common pathophysiological feature of various stress-related diseases. Genes regulating HPA axis activity, including the glucocorticoid receptor (GR), are implicated in stress-related psychopathologies like BD. The cell cycle gene SKA2, an interaction partner of the GR, facilitates the receptor's nuclear translocation in peripheral cells. Intriguingly, single nucleotide polymorphisms (SNPs) and DNA methylation within SKA2, as well as alterations in its gene expression, have been repeatedly associated with PTSD and suicide risk in human patients. However, the specific role of SKA2 in neurons, which are non-replicating post-mitotic cells, in relation to glucocorticoid dysregulation and stress-related psychiatric disorders, including BD, remains largely unexplored. In this project, we aim to investigate the function of SKA2 in the central nervous system (CNS) of both mice and humans, assessing its relevance to stress-related psychiatric disorders, including BD. This research will be instrumental in guiding the development of novel treatment strategies for these conditions.